Chronic Headaches
By Jamie Camp
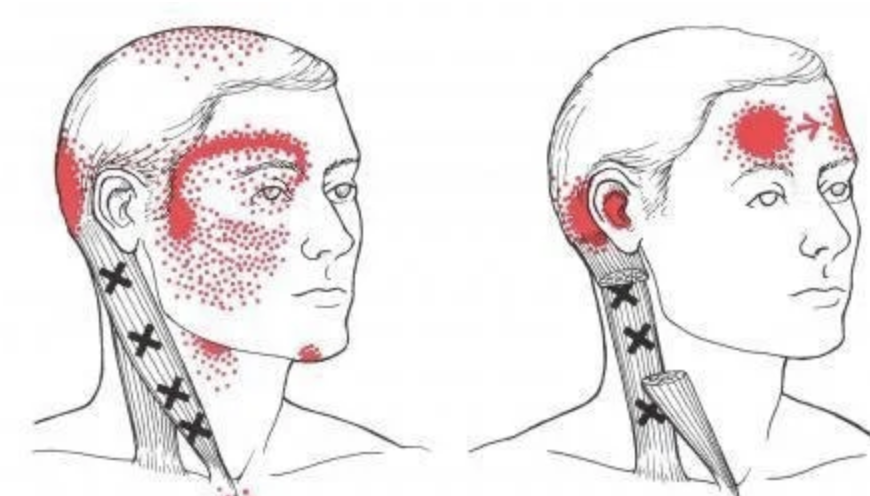
Headache referral patterns
Chronic Headaches case study and literature review
Saw a longtime rugby player two weeks ago. Their complaint was years of chronic migraines, and constant headaches. Headaches since first concussion around age 12. They’ve tried everything: therapy, botox, medication twice a day and migraine medication. The headaches were accompanied by dizziness, nausea, flashes & light sensitivity. The past injury list was long: concussions, broken jaw, broken ribs, broken ankles, and the list goes on. #rugby
To make matters more interesting, one of the concussions was accompanied by a forehead laceration requiring stitches.
On assessment, left side neck rotation was limited in standing. Hip mobility was limited. Using Neurokinetic therapy testing, their forehead scar was facilitated for another inhibited eyebrow scar. On testing through core stability, Transversus abdominis was inhibited by a facilitated Right piriformis (affecting overall stability and hip mobility). Their neck rotation was playing tug of war as well, likely contributing to headaches. Left sternocleidomastoid (SCM) was overworking for the same muscle on the right side. Fun fact, your SCM rotates your head to the opposite side, and limits rotation to the same side.
We used soft tissue work to release the overworking muscles and bring the underworking muscles back online. They laughed on the way out and said those findings were interesting, as they often hold their forehead scar to try and relieve their headaches. Came back for a followup this week (two weeks later, having done some homework to reinforce what we found) and reported that constant headaches were usually 8/10, and went down to 1/10 with periods of no headache. They had one migraine which is less frequent than usual. I’ll take it. This the first layer of the onion but hopefully also the first step to restoring headache free living. Next few treatments - support that progress with some neurofunctional acupuncture, more soft tissue work, functional movement.
A few clinical pearls:
This player’s lack of left neck rotation was a big clue- functional movement while someone is standing up against gravity can tell you a lot about what is holding on for dear life.
Start with core testing - if your pelvis isn’t stable, all bets are off.
Ensure medical imaging to rule out anything sinister - we always have to have our spidey sense turned on in this field
Scars are neurologically active - ie can really throw a wrench into the mix and disrupt normal tone (think C-section scars, etc)
Ankle fractures change how your foot loads everything else up the chain to the top of your head #whatthefoot - We can’t blame everything on them but they have a lot to atone for.
Past medical history matters - injury lives in your nervous system and the longer it’s been there, the more corrosive it is.
In earlier civilizations, trepanization (drilling holes in the skull) was performed because of the belief that this would release demons that had entered into the skull and had to be released, if headache relief was to result. So at least we’ve come a little ways since then. Anatomy for the win.
Headaches are kind of a big deal. The prevalence of tension headaches are estimated to affect 78-90% of the general population at one time or another in their lives.
There is a relationship between headaches and migraines: a Danish study showed that 83% of migraine sufferers experience episodes of muscle tension headache and that conversely 23% of the severe muscle tension headache sufferers had migraines.
Tension and stress are not the same.
A systematic review summarized the correlation between temporomandibular/joint disorders and tension headaches. Correlations were found between headaches and EMG values of the frontalis muscle (where our player’s scar is). There are also correlations between the craniomandibular structures (jaw, skull, teeth and muscles) and noted that “when the muscle groups are unbalanced, physiological changes lead to manifestations that include acute and chronic tension types of headaches”. Jaw fracture = temporomandibular dysfunction.
Other systems don’t get out unscathed either; proprioception is affected when muscle tone is altered. These facial/skull muscles and structures are closely related to neural structures and can interact with our central nervous system as well. Headache relief comes from lowering resting electrical activity in these muscles; specifically the elevator (temporalis and masseter) and the depressor (anterior digastric) muscles and improving symmetry. Chronic tension can also be referred from dysfunctional tone in posterior cervical, head, and shoulder muscles. When there is repeated noxious (painful) stimuli, your brain gives that more neural connections to pay attention to it = chronic pain and central sensitization. Whiplash, jaw trauma, facial trauma, etc. Svensson et al described the overlap between TMJ dysfunction and tension-type headaches with regards to sensitization of central and peripheral pain pathways and dysfunction in modulatory systems. The local microenvironment around trigger points has also been described in the literature, whereby the levels or neuroactive substances are increased affecting the nervous system.
A systematic review concluded that Physiotherapy treatment based on manual therapy, specifically the combination of soft tissue techniques and structural techniques (manipulation), in addition to craniocervical flexion exercises, achieves positive outcomes in pain intensity and frequency, disability, impact of headache, quality of life, and craniocervical range of motion in adults with tension type headaches.
Correcting motor compensations using techniques like Neurokinetictherapy combined with soft tissue work can problem solve this dysfunction efficiently, improving muscle tone, proprioception, motor control range of motion, etc. It essentially ensures that no muscle group is working above it’s paygrade and screaming at you. At Shift, these techniques are the basis for our assessment and treatments. #getassessed
References:
Cooper BC, Kleinberg I. Relationship of temporomandibular disorders to muscle tension-type headaches and a neuromuscular orthosis approach to treatment. Cranio. 2009 Apr;27(2):101-8. doi: 10.1179/crn.2009.016. PMID: 19455921.
Svensson P. Muscle pain in the head: overlap between temporomandibular disorders and tension-type headaches. Curr Opin Neurol. 2007 Jun;20(3):320-5. doi: 10.1097/WCO.0b013e328136c1f9. PMID: 17495627.
Cumplido-Trasmonte C, Fernández-González P, Alguacil-Diego IM, Molina-Rueda F. Manual therapy in adults with tension-type headache: A systematic review. Neurologia (Engl Ed). 2021 Sep;36(7):537-547. doi: 10.1016/j.nrleng.2017.12.005. Epub 2020 Apr 7. PMID: 34537167.